ARTICLE TOOLS
Research Article - (2023) Volume 14, Issue 1
Abstract
Stylosanthes fruticos, a perennial plant has been revered in ayurveda medicine for generations. The aim of the present study was to determine the antidiarrheal activity of ethanolic extract of S. fruticos (EESF), utilizing castor oil-induced, magnesium sulphate induced diarrhoea and castor oil-induced enteropooling in mice. The presence of alkaloids, carbohydrates, flavonoids, steroids, and phenols was discovered by phytochemical screening of EESF. At 25 mg/kg of dosage, the EESF provided considerable significant (p<0.05) inhibition on castor oil-induced diarrhea, magnesium sulphate induced diarrhea and castor oil induced enteropooling. From the findings, it was evident that EESF had dose-dependent antidiarrheal effects in all treatment groups, and the results were also well comparable with loperamide (3 mg/kg) as the reference drug.
Keywords
Stylosanthes fruticosa, Diarrhea, Ethanolic extract, Castor oil, Magnesium sulphate
Introduction
According to estimates, India has a rich history of medicinal plants, with 7,500 out of 17,000 higher plant species being therapeutic plants), which is more than any other country in the world in relation to the country’s current flora (Kala CP, et al., 2006). As a result, there has been a recent surge in demand for herbal treatments, resulting in increased demand for medicinal plants and their bioactive components, which are being studied scientifically (Velázquez C, et al., 2012). Recently, medical research has begun to examine the comprehensive chemical screening for a wide range of therapeutic plants, as well as its various phytoconstituents. Every year, approximately one lakh secondary metabolites are extracted from approximately 50,000 plant species, with 4,000 novel secondary metabolites isolated from a wide range of plant species. These phytoconstituents have been used for diversed applications, including human healthcare (as antioxidants and pharmaceuticals), numerous industries (as colours, tastes, and fragrances), and agriculture (as pesticides and pheromones) (Derebe D, et al., 2018; Gómez-Galera S, et al., 2007; Brinda P, et al., 1981; Dulara BK, et al., 2019). Conversely, traditional healers regularly utilize antidiarrheal medicinal plants, although further study on medicinal plants in the management of diarrheal illnesses is urgently needed. As a result, international organizations such as the World Health Organization (WHO) have promoted research into the management and prophylaxis of diarrhoeal disorders utilizing conventional medical techniques (Venu C, et al., 2016; Saralaya MG, et al., 2010; Jabri MA, et al., 2016). There is a wealth of epidemiological study data on global acute diarrheal illness, which is one of the leading reasons of morbidity and mortality, especially underweight children, which is a serious concern in developing countries (Snyder JD and Merson MH, 1982; Ganapaty S, et al., 2013).
Acute diarrhea is the most prevalent type of diarrhea, followed by chronic diarrhea. And over 90% of instances of acute diarrhea are caused by infectious organisms; such symptoms are frequently accompanied by vomiting, fever, and stomach discomfort also results by disruptions in the intestine’s secretory and absorptive activities, result in an increased frequency (3 or more times/day), flow rate, and/or volume of faeces. Medication, hazardous ingestions, ischemia, and other diseases account for the remaining 10%. Even though viral and bacterial agents are important pathogens, Shigella flexneri, S. aureus, E.coli, rotavirus and S. typhi are the most common pathogens responsible for diarrhea in young children and adults (Hodges K and Gill R, 2010; Brijesh S, et al., 2011; Umer S, et al., 2013; Omori EO, et al., 2012; Naher S, et al., 2019).
Management of diarrhea includes antimotility medications. As a result, it is critical to discover and assess accessible natural medications as substitutes to commonly used antidiarrheal pharmaceuticals, which are not always devoid of side effects. Stylosanthes fruticosa (Family Fabaceae) was commonly known as African stylo, Ladinala, Wal-nanu, Wildlucerine, Shrubby pencil flower. It is woody plant with copious branches as shown in Figure 1, ascending or under shrub, and also is a perennial that can act as an annual in the subtropics and found in Sudan, Nigeria, Kenya, Uganda, Tanzania, Zambia, Mozambique, Zimbabwe, South Africa, and southern India (Sandosh AT, et al., 2013; Peter PJ, 2012).
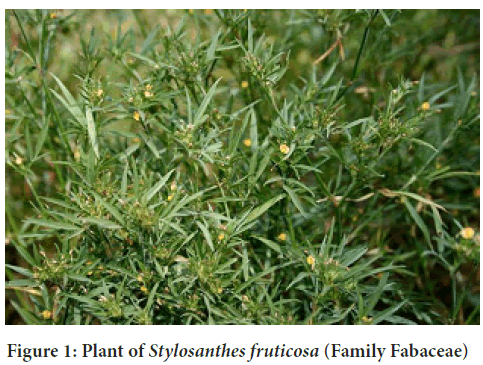
Figure 1: Plant of Stylosanthes fruticosa (Family Fabaceae)
In the study reported by Venkatesh P, et al., 2019 ethanolic extract of Stylosanthes fruticosa, have been inferred the presence of phytochemicals and reported that 800 mg/kg of extract has shown significant analgesic activity than other doses when studied on mice by hot plate method using reference drug as aspirin. Kumamanan R, et al., 2014 confirmed potential anthelminthic activity of Stylosanthes fruticosaupon comparative study along with Indigofera linnae at a concentration of 500 mg/ml using albendazole as reference standard and distilled water as control. Paul JP, et al., 2012 studied the efficiency of S. fruticosa crude plant extract on gram positive bacteria (Bacillus cereus, Staphylococ cus faecalis, S. auerus) and gram negative bacteria (Proteus vulgaris, Sal- monella lyphimurium, Escherichia coli, Klebsiella pneumoniae and Pseudo monas aeurginosa). The effectiveness of acetone, chloroform and ethanolic extract of Stylosanthes fruticosaon antibacterial activity was determined and was clearly indicated that ethanolic extract showed high degree of inhibition when compared with other extract using chloramphenicol (30 µg/ disc) as reference standard (Evans WC, 1989). After a thorough search, no evidence of antidiarrheal effect on S. fruticosa was found; hence the goal of this study was to evaluate the antidiarrheal activity of an ethanolic extract of Stylosanthes fruticosa leaves.
Materials and Methods
Materials
Fresh leaves of Stylosanthes fruticosa were collected from the vicinity of Sri Krishnadevaraya University premises and was authenticated by Prof. B. Ravi Prasad Rao, Head and Director, S.K.U (Herbarium) Department of Botany, Ananthapurmau, India with voucher no.57419 (SKU) dated 22- 02-202.
Loperamide hydrochloride was supplied by Micro Labs Ltd. in Bangalore. All additional chemicals and solvents were bought locally and were of biological and analytical quality.
Preparation of extract
Fresh leaves of Stylosanthes fruticosa were picked on the SK University campus. The samples were washed with running tap water for 10 minutes to remove dirt particles and adhering material. After that, the samples were thoroughly washed with distilled water. The leaves were then cut and dried for one week in the shade at room temperature before being ground into powder. The powder (42 g) was extracted with ethanol for 5-6 hours using a soxhlet apparatus. The extract was filtered using Whatmann filter paper No: 41 with 2 g sodium sulphate to remove the sediment and traces of water in the filter. Prior to filtering, the filter paper and sodium sulphate are wetted with 100% alcohol. The filtrate is then concentrated.
Preliminary phytochemical screening
Stylosanthese fruticosa ethanolic extract was tested for the presence of several phytoconstituent classes like alkaloids, glycosides, saponins, tannins, flavanoids and steroids that can be inferred by the characteristic colour change of various reagents used in accordance with the standard procedures narrated by Harbone and Trease (Singh B, et al., 2003; Amoo SO, et al., 2009; Shiramane RS, et al., 2011).
Antidiarrhoeal activity
Experimental animals: Male albino rats weighing 150-250 gms were procured from Sri Venkataeswara Enterprises, Bangalore. Animals were cared for in accordance with the NIN animal user instructions and are acclimated for 10 days to our animal housing, which is kept at a temperature of 22°C to 12°C. The animal was kept on a 12-hour light/12-hour dark cycle. Five creatures are kept in each cage, which measures 41 cm in length, 28 cm in breadth, and 14 cm in height. Paddy husk was used for bedding, and on very different days, the bedding was changed and properly cleansed with water and Domex, a disinfectant and detergent. A regular pellet diet obtained from Sai Durga Feeds and Foods Bangalore was provided to the rats.
Acute toxicity testing: Acute toxicity testing was performed in accordance with the OECD 425 Guidelines. Female Swiss albino mice were fasted for 4 hours before being orally loaded with 2000 mg/kg of the extract. The mouse was then rigorously watched for physical or behavioral changes within 24 hours, with specific emphasis on the first 4 hours. Based on the findings from the first animal, four additional female mice were recruited and starved for four hours. The animals were next given a single dosage of 2000 mg/kg, followed by comparable stringent observation. Such monitoring was extended for another 14 days to look for any evidence of toxicity.
Study protocol
Castor oil induced diarrhea: Male albino rats were separated into four groups of five (n=5). All rats were fasted for 18 hours, allowed unrestricted access to water during the experiment, and administered castor oil orally (p.o) via orogastric cannula for induction of diarrhea. In group 1 (control group), each rat was given normal saline solution at a dosage of 1 ml/100 g according to the weight using orogastric cannula. In group 2,3 and 4 each rat was given EESF at a dosage of 25, 50 and 100 mg/kg according to body weight using orogastric cannula in the form of suspension containing 0.5% Sodium Carboxy Methyl Cellulose (SCMC) as suspending agent. In group 5, each rat was given reference drug, loperamide 3 mg/kg according to the weight using orogastric cannula in form of suspension containing 0.5% SCMC as suspending agent. The mice were kept separately in individual cages on fresh white Whatman filter paper that was changed hourly. Frequency of diarrhoea was assessed every four hour. The control group’s total amount of diarrhea faeces was represented as 100% (Shoba FG and Thomas M, 2001; Robert A, et al., 1976).
Antidiarrhoeal activity was calculated as % inhibition, which shall be computed as follows formula.
% Inhibition=Mean weight of stool of control animals-Mean weight of stool of EESF treated animals × 100/Mean weight of stool of control animals
Magnesiun sulphate-induced diarrhea: Male albino rats were separated into four groups of five (n=5). All rats were fasted for 18 hours, allowed unrestricted access to water during the experiment, and administered magnesium sulphate at a dosage of 2 mg/kg orally (p.o) via orogastric cannula for induction of diarrhoea. After 30 minutes, in group 1 (control group), each rat was given normal saline solution at a dosage of 1 ml/100 g according to the weight using orogastric cannula. In group 2, 3 and 4, each rat was given EESF at a dosage of 25, 50 and 100 mg/kg according to body weight using orogastric cannula in the form of suspension containing 0.5% SCMC. In group 5, each mice was given reference drug, loperamide 3 mg/kg according to the body weight using orogastric cannula in form of suspension containing 0.5% SCMC. Each mouse was kept separately in individual cages on fresh white Whatman filter paper that was changed hourly. Frequency of diarrhoea was assessed every four hour. The control group’s total amount of diarrhoea faeces was represented as 100%. Each group’s activity was given as a percentage inhibition (%) with the previously mentioned formula.
Castor oil induced enteropooling: Thirty mice were selected at random, starved for 18 hours before to the study, and randomly allocated to five groups of six mice each. Group 1 served as a control, while Group 2, 3 and 4 administered 25, 50 and 100 mg/kg dosages of EESF, respectively, and Group 5 received loperamide solution (3 mg/kg). After 30 minutes administration of EESF extract, each group’s animals were given 0.3 ml of castor oil orally. Then the mice’s are sacrificed by cervical dislocation. Thirty minutes later, whole length of the small intestine taken directly from the pylorus to the caecum and the contents of intestine were collected and measured (Derebe D, et al., 2018; Doherty NS, 1981).
Results and Discussion
Screening for phytochemical constituents
Phytochemical studies of ethanolic extract of S. fruticosa leaves were performed and represented in Table 1. From the carbohydrate and glycoside qualitative phytochemical tests inference, it is revealed that it produces an excellent distinctive color and precipitate in all respective tests. Presence of phenolic compounds and flavonoids was also confirmed by significant characteristic colour. Slight presence of saponins, phytosterols was found with a mild colour, and also no color confirms the absence of proteins and alkaloids for the respective tests.
| Chemical constituents | Tests | Result |
|---|---|---|
| Alkaloids | Mayer’s test | Negative |
| Dragendroff’s test | Negative | |
| Wagner’s test | Negative | |
| Hager’s test | Negative | |
| Carbohydrates | Molisch’s test | Positive |
| Benedict’s test | Positive | |
| Fehling test | Positive | |
| Glycosides | Libermann-Burchard test | Negative |
| Modified Borntrager test | Negative | |
| Legals test | Negative | |
| Saponins | Foam test | Positive |
| Phytosterols | Salkowski test | Positive |
| Libermann Burchard test | Positive | |
| Flavonoids | Alkaline reagent test | Positive |
| Lead acetate test | Positive | |
| Shinoda test | Positive | |
| Phenolic acids and tannins | Ferric chloride test | Positive |
| Gelatin test | Positive | |
| Proteins and amino acids | Xanthoproteic test | Negative |
| Ninhydrin test | Negative | |
| Biuret test | Negative |
Table 1: Phytochemical screening of EESF (Ethanolic extract of S.fruticos)
Acute toxicity studies
EESF oral dosing was determined to be safe at a dosage of p.o. 2000 mg/kg. There were no symptoms of toxicity. However, EESF at 5 g/kg induced delayed animal locomotion and lowered aggression, as well as altered touch and pain sensitivity, there were no detrimental behavioral changes as a result of excitation, respiratory distress, convulsions, or coma which are all possible symptoms. Up to 14 days, no death was recorded. As a result, the median LD50 EESF levels were then more than 2000 mg/kg body weight. Therefore, for this study, dosages of 25, 50, and 100 mg/kg body weight were used. All tests were conducted in-vivo.
Castor oil induced diarrhea
The EESF was discovered to be efficient against castor oil induced diarrhea test at dosages of 25, 50, and 100 mg/kg body weight. On administration of EESF extract at 25, 50 and 100 mg/kg dosages in mice, the number of watery fecal drops are i.e.,8.3 ± 0.67, 12.3 ± 0.45 and 15.2 ± 0.83 and amount of watery fecal drops are 2.44 ± 0.19, 3.62 ± 0.19 and 4.54 ± 0.18 respectively for group 2, 3 and 4 animals. The overall number of watery stool and amount of fecal drops was significantly reduced in comparison to the control group (i.e., 21.6 ± 1.67 and 6.44 ± 0.32).The impact of dosages of EESF was comparable with the reference drug (loperamide 3 mg/kg) depicted in Table 2 with percentage inhibition of diarrhea of 62.11 (25 mg/kg), 43.78 (50 mg/kg) and 29.50 (100 mg/kg) respectively and conclude that EESF has shown antidiarrhoeal activity in dose dependent manner.
| Group | Dose (mg/kg) | Mean number of fecal drops (n=5) | Mean weight of feaces (g) (n=5) | Percentage inhibition (%) |
|---|---|---|---|---|
| 1 | - | 21.6 ± 1.67 | 6.44 ± 0.32 | - |
| 2 | 25 | 8.3 ± 0.67* | 2.44 ± 0.19* | 62.11 |
| 3 | 50 | 12.3 ± 0.45* | 3.62 ± 0.19* | 43.78 |
| 4 | 100 | 15.2 ± 0.83* | 4.54 ± 0.18* | 29.5 |
| 5 | Loperamide | 5.2 ± 0.84* | 0.63 ± 0.05* | 90.21 |
Note: Values are depicted as mean ± SD, *Statistically significant values (p<0.05) in comparison with the control group
Table 2: Effect of EESF (Ethanolic extract of S. fruticos) on castor oil induced diarrhea
Mg SO4 induced diarrhea
The EESF was discovered to be efficient against Mg SO4 induced diarrhea test at dosages of 25, 50, and 100 mg/kg body weight. At dosages of 25, 50 and 100 mg/kg, the EESF extract considerably decreases the number of watery fecal drops (i.e., 7.24 ± 0.43, 8.7 ± 0.33 and 10.8 ± 0.44) and amount of watery fecal drops (i.e., 2.14 ± 0.01, 3.06 ± 0.01 and 3.98 ± 0.08) upon administration of magnesium sulphate respectively in comparison of control at p<0.05. The overall number of watery stool and amount of fecal drops was significantly reduced in comparison to the control group (i.e., 19.1 ± 0.22 and 5.56 ± 0.21).The impact of dosages of EESF was comparable with the reference drug (loperamide 3 mg/kg) depicted in Table 3with percentage inhibition of diarrhea of 61.43 (25 mg/kg), 44.92 (50 mg/kg) and 28.41 (100 mg/kg) respectively and conclude that EESF has shown antidiarrhoeal activity in dose dependent manner.
| Group | Dose (mg/kg) | Mean number of fecal drops (n=5) | Mean weight of feaces (g) (n=5) | Percentage inhibition (%) |
|---|---|---|---|---|
| 1 | - | 19.1 ± 0.22 | 5.56 ± 0.21 | - |
| 2 | 25 | 7.24 ± 0.43 | 2.14 ± 0.01* | 61.43 |
| 3 | 50 | 8.7 ± 0.33 | 3.06 ± 0.01* | 44.92 |
| 4 | 100 | 10.8 ± 0.44 | 3.98 ± 0.08* | 28.41 |
| 5 | Loperamide | 4.18 ± 0.23 | 0.73 ± 0.03* | 86.83 |
Note: Values are depicted as mean ± SD, *Statistically significant values (p<0.05) in comparison with the control group
Table 3: Effect of EESF (Ethanolic extract of S. fruticos) on Mg SO4 induced diarrhoea
Castor oil induced enteropooling
The EESF was found to have remarked anti-enteropooling activities in castor oil induced experimental animals depicted in Table 4. In control group of animals, the intestinal contents volume was found to be 2.99 ±0.17 ml. Loperamide (3 mg/kg), a typical medication, was also very effective in decreasing the intestinal contents volume to 0.29 ml as compared with control (p<0.05) Substantial suppression of intestinal contents by 0.67, 0.52 and 0.45 ml for 100 mg/kg, 50 mg/kg and 25 mg/kg in comparison with control group indicates the values are statistically significant at p<0.05 level in a dose dependent manner. The EESF significantly reduced intestinal volume content (p<0.01) at doses of 25 mg/kg, 50 mg/kg and 100 mg/kg.
| Group | Dose (mg/kg) | Volume of intestinal contents (ml) |
|---|---|---|
| 1 | - | 2.99 ± 0.17 |
| 2 | 25 | 0.45 ± 0.17* |
| 3 | 50 | 0.52 ± 0.17* |
| 4 | 100 | 0.67 ± 0.17* |
| 5 | Loperamide | 0.29 ± 0.17* |
Note: Values are depicted as mean ± SD, *Statistically significant values (p<0.05) in comparison with the control group
Table 4: Effect of EESF (Ethanolic extract of S. fruticos) on castor oil induced enteropooling
Conclusion
The present study determines that EESF at doses of 25 mg/kg, 50 mg/kg and 100 mg/kg body weight of mice produces dose dependent and significant (p<0.05) values against castor oil induced and magnesium sulphate induced diarrhoea and castor oil induced enteropooling in comparison with reference drug as loperamide. Due to its antidiarrheal properties, S. fruticosa has the capability to alleviate GI problems such as diarrhoea. More research is needed to back up the above claim and determine the actual molecular mechanisms involved in this plant’s antidiarrheal effect.
Acknowledgment
The authors would like to thank Raghavendra Institute of Pharmaceutical Education and Research, Ananthapuramu for their kind support during animal studies.
Ethical Approval
Local Institutional Animal Ethical Committee of RIPER has been obtained for the purpose of control and supervision of experiments on animals for the present study. (CPCSEA) (Approval no: 878/ac/05/CPCSEA/12/21).
References
- Kala CP, Dhyani PP, Sajwan BS. Developing the medicinal plants sector in northern India: Challenges and opportunities. J Ethnobiol Ethnomed. 2006; 2(1): 1-5.
- Velázquez C, Calzada F, Bautista M, Gayosso JA. Management of secretory diarrhea. Curr Concepts Colon Disord. 2012.
- Derebe D, Abdulwuhab M, Wubetu M, Mohammed F. Investigation of the antidiarrheal and antimicrobial activities of 80% methanolic leaf extract of Discopodium penninervum (hochst.). Evid Based Complement Alternat Med. 2018.
[Crossref] [Google scholar] [Pubmed]
- Gómez-Galera S, Pelacho AM, Gené A, Capell T, Christou P. The genetic manipulation of medicinal and aromatic plants. Plant cell rep. 2007; 26(10): 1689-1715.
[Crossref] [Google scholar] [Pubmed]
- Brinda P, Sasikala B, Purushothaman KK. Pharmacognostic studies on Merugan kilanzhu. Bull med-ethno-bot res. 1981; 8: 1-3.
- Dulara BK, Godara P, Barwer N. In-vivo and in-vitro phytochemical GC-MS analysis of volatile constituents of Andrographis paniculata (Burm. f.) Nees. J Pharm Innov. 2019; 8: 255-261.
- Venu C, Ramanjaneyulu K, Reddy SN, Laxmi V, Alla B. Evaluation of antidiarrhoeal activity of ethanolic extracts of Pithecellobium dulce on castor oil-induced diarrhoea in albino wistar rats. Discovery. 2016; 52: 1494-1496.
- Saralaya MG, Patel P, Roy MP, Patel AN. Research article antidiarrheal activity of methanolic extract of Moringa oleifera Lam roots in experimental animal models. Int J Pharm Res. 2010; 2(2): 25-29.
- Jabri MA, Rtibi K, Ben-Said A, Aouadhi C, Hosni K, Sakly M, et al. Antidiarrhoeal, antimicrobial and antioxidant effects of myrtle berries (Myrtus communis L.) seeds extract. J Pharm Pharmacol. 2016; 68(2): 264-274.
[Crossref] [Google scholar] [Pubmed]
- Snyder JD, Merson MH. The magnitude of the global problem of acute diarrhoeal disease: A review of active surveillance data. Bull World Health Organ. 1982; 60(4): 605.
[Google scholar] [Pubmed]
- Ganapaty S, Ramaiah M, Yasaswini K, Nuthakki VK, Harikrishnareddy D. Quantitative estimation of phytoconstituents and in vitro antioxidant standardization of whole plant of Dendrobium ovatum (L.) Kraenzl. J pharmacogn phytochem. 2013; 4(9): 2291-2297.
- Hodges K, Gill R. Infectious diarrhea: Cellular and molecular mechanisms. Gut microbes. 2010; 1(1): 4-21.
[Crossref] [Google scholar] [Pubmed]
- Brijesh S, Tetali P, Birdi TJ. Study on effect of anti-diarrheal medicinal plants on enteropathogenic Escherichia coli induced interleukin-8 secretion by intestinal epithelial cells. Altern Med Stud. 2011; 1(1): e16.
[Crossref] [Google scholar] [Pubmed]
- Umer S, Tekewe A, Kebede N. Antidiarrhoeal and antimicrobial activity of Calpurnia aurea leaf extract. BMC Complement Altern Med. 2013; 13(1): 1-5.
[Crossref] [Google scholar] [Pubmed]
- Omori EO, Calistus O, Mbugua PK, Okemo PO. Ethnobotanical identification and anti-microbial evaluation of some anti-diarrhoreal plants used by the Samburu community, Kenya. Malays J Microbiol. 2012; 8(2): 68-74. [Crossref]
- Naher S, Aziz M, Akter M, Rahman SM, Sajon SR, Mazumder K. Anti-diarrheal activity and brine shrimp lethality bioassay of methanolic extract of Cordyline fruticosa (L.) A. Chev. leaves. Clin Phytosci. 2019; 5(1): 1-6.
- Sandosh AT, Peter PJM, Raj YJ. Phytochemical analysis of Stylosanthes fruticosa using UV-VIS, FTIR and GC-MS. Res J Chem Sci. 2013; 3(11): 14-23. [Crossref]
- Peter PJ. GC-MS analysis of bioactive components on the leaves extract of Stylosanthes fruticosa-a potential folklore medicinal plant. Int J Phytopharm. 2012; 2(3).
[Crossref] [Google scholar]
- Venkatesh P, Pravallika H, Sravani L, Kumar AA, Narasimhulu MK, Kalarani H. Screening of analgesic activity of ethanolic extract of Stylosanthes fruticosa by hot plate method. J Pharma Res. 2019; 8(4): 191-193.
- Kumanan R, Sridhar C, Jayaveera KN, Sudha S. Comparative study of Stylosanthes fruticosa and Indigofera linnae for anthelmintic activity. Indian J Pharm Sci. 2014; 2(3): 1237.
- Paul JP, Venkatesan M, Yesu JR. The antibacterial activity and phytochemicals of the leaves of Stylosanthes fruticosa Linn. Intl Journ of Phytopharm Res. 2012; 3(4): 96-106.
- Evans WC. Trease and Evans pharmacognosy, 15th. London: Baillière Tindall. 1989.
- Singh B, Bani S, Gupta DK, Chandan BK, Kaul A. Anti-inflammatory activity of ‘TAF’an active fraction from the plant Barleria prionitis Linn. J Ethnopharmacol. 2003; 85(2-3): 187-193.
[Crossref] [Google scholar] [Pubmed]
- Amoo SO, Finnie JF, van Staden J. In vitro pharmacological evaluation of three Barleria species. J Ethnopharmacol. 2009; 121(2): 274-277.
[Crossref] [Google scholar] [Pubmed]
- Shiramane RS, Biradar KV, Chivde BV, Shambhulingayya HM, Goud V. In-vivo antidiarrhoeal activity of ethanolic extract of Delonix regia flowers in experimental induced diarrhoea in wistar albino rats. Int J Res Pharm Chem. 2011; 1(3): 2231-2781.
- Shoba FG, Thomas M. Study of antidiarrhoeal activity of four medicinal plants in castor-oil induced diarrhoea. J Ethnopharmacol. 2001; 76(1): 73-76.
[Crossref] [Google scholar] [Pubmed]
- Robert A, Nezamis JE, Lancaster C, Hanchar AJ, Klepper MS. Enteropooling assay: A test for diarrhea produced by prostaglandins. Prostaglandins. 1976; 11(5): 809-828.
[Crossref ] [Google scholar] [Pubmed ]
- Doherty NS. Inhibition of arachidonic acid release as the mechanism by which glucocorticoids inhibit endotoxin-induced diarrhoea. Br J Pharmacol. 1981; 73(2): 549.
[Crossref] [Google scholar] [Pubmed]
Author Info
Gayathri S1*, Jayanth Reddy K1, Samuel Y1, Vyshnavi C1, Savithri D2, Pavithra H2, Nikhitha K2 and Soma Sekhar Reddy K22Department of Pharmacology, Raghavendra Institute of Pharmaceutical Education and Research, Andhra Pradesh, India
Citation: Gayathri S: Anti-Diarrheal Activity of Ethanolic Extract of Stylosanthes fruticosa Leaves in Mice
Received: 02-Dec-2022 Accepted: 27-Dec-2022 Published: 03-Jan-2023, DOI: 10.31858/0975-8453.14.1.6-10
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Psychometric properties of the World Health Organization Quality of life instrument, short form: Validity in the Vietnamese healthcare context Trung Quang Vo*, Bao Tran Thuy Tran, Ngan Thuy Nguyen, Tram ThiHuyen Nguyen, Thuy Phan Chung Tran SRP. 2020; 11(1): 14-22 » doi: 10.5530/srp.2019.1.3
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- Deuterium Depleted Water as an Adjuvant in Treatment of Cancer Anton Syroeshkin, Olga Levitskaya, Elena Uspenskaya, Tatiana Pleteneva, Daria Romaykina, Daria Ermakova SRP. 2019; 10(1): 112-117 » doi: 10.5530/srp.2019.1.19
- Dental Development between Assisted Reproductive Therapy (Art) and Natural Conceived Children: A Comparative Pilot Study Norzaiti Mohd Kenali, Naimah Hasanah Mohd Fathil, Norbasyirah Bohari, Ahmad Faisal Ismail, Roszaman Ramli SRP. 2020; 11(1): 01-06 » doi: 10.5530/srp.2020.1.01
- Manilkara zapota (L.) Royen Fruit Peel: A Phytochemical and Pharmacological Review Karle Pravin P, Dhawale Shashikant C SRP. 2019; 10(1): 11-14 » doi: 0.5530/srp.2019.1.2
- Pharmacognostic and Phytopharmacological Overview on Bombax ceiba Pankaj Haribhau Chaudhary, Mukund Ganeshrao Tawar SRP. 2019; 10(1): 20-25 » doi: 10.5530/srp.2019.1.4
- A Review of Pharmacoeconomics: the key to “Healthcare for All” Hasamnis AA, Patil SS, Shaik Imam, Narendiran K SRP. 2019; 10(1): s40-s42 » doi: 10.5530/srp.2019.1s.21
- A Prospective Review on Phyto-Pharmacological Aspects of Andrographis paniculata Govindraj Akilandeswari, Arumugam Vijaya Anand, Palanisamy Sampathkumar, Puthamohan Vinayaga Moorthi, Basavaraju Preethi SRP. 2019; 10(1): 15-19 » doi: 10.5530/srp.2019.1.3






