Patient Education and Consent
Obtain informed consent from the patient or guardian. The patient should be informed in advance that the procedure involves placing a tube and draining the bladder through the abdominal wall.
Patients should be instructed on how to care for the catheter and empty and change drainage bags (eg, from a leg bag during daytime use to a larger drainage bag for overnight use). The suprapubic catheter exit site should be washed daily with soap and water and may be covered with gauze. If not otherwise contraindicated, patients should be instructed to drink plenty of fluids.
Patients should be instructed to seek immediate medical attention for catheter replacement if the catheter becomes dislodged. The tract can close very quickly, requiring suprapubic cystostomy to be performed again, if the suprapubic tube is not urgently replaced.
Equipment
A number of percutaneous suprapubic cystostomy kits are on the market. All are based on the same principle. It should be kept in mind that if a suprapubic catheter kit is not available during an emergency situation that calls for urgent bladder drainage, any device suitable for central venous access can be placed suprapubically by using the Seldinger technique. [3]
Materials used for suprapubic cystostomy include the following (other materials, if equivalent, can be easily substituted):
-
Sterile gloves
-
Face mask with protective shield
-
Clippers/shaver (to remove hair at the suprapubic site)
-
Sterile towels (4) or drapes
-
Antiseptic solution/applicators (eg, 3 ChloraPreps; CareFusion, Leawood, KS)
-
Marking pen
-
1% lidocaine (5 mL) and 0.25% bupivacaine (5 mL) in a Luer-Lok syringe
-
22-gauge, 7.75-cm spinal needle tip (some use 18- and 25-gauge needles)
-
Scalpel with a No. 11 blade
-
10 mL of sterile water in a Luer-Lok syringe (to inflate the catheter balloon)
-
Skin tape or 3-0 nylon suture on a curved needle (to secure the catheter loosely to the skin)
-
Adson tissue forceps, 1 × 2 teeth, 4.7 in.
-
Baumgartner needle holder, 5.5 in.
-
4×4 inch drain gauze (2) or drain sponges
-
Tube-securing device (eg, Statlock, Bard Medical Division, Covington, GA; or Cath-Secure, M.C. Johnson, Fort Myers, FL)
-
Catheter drainage bag
-
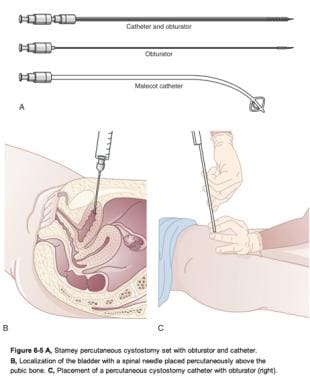
Suprapubic catheter kit – Many choices exist, all of which have their own slight variations; examples include the Rutner percutaneous suprapubic balloon catheter set, the Cook Peel-Away Sheath Introducer, and the Stamey Percutaneous Malecot suprapubic catheter set (see the image below), all made by Cook Medical (Bloomington, IN)
Patient Preparation
Anesthesia
Some physicians desire patients undergoing suprapubic cystostomy placement to receive parenteral analgesia, with or without sedation. To ensure patient and practitioner safety during this invasive procedure, procedural sedation and analgesia may be considered in all patients who are uncooperative or agitated.
Local anesthesia should be used for a percutaneous suprapubic cystostomy. Light sedation may also be beneficial for patient comfort. An example of an appropriate preparation would be a 1:1 formulation of lidocaine 1% 5 mL and bupivacaine 0.25% 5 mL, for a total of 10 mL. Many other formulations compositions would serve equally well as a local anesthetic. With a 22-gauge needle tip, infiltrate the superficial and subcutaneous tissue down to the fascia, approximately 2 fingerbreadths above the pubic symphysis.
Positioning
During percutaneous suprapubic cystostomy placement under cystoscopic guidance, the patient could be either supine, if a flexible cystoscope is being used, or in the dorsal lithotomy position, if a rigid cystoscope is being used. If the urethra can be cannulated, the cystoscope allows observation of the dome of the bladder during the procedure, enabling visual confirmation of percutaneous entry into the bladder.
For any of the other percutaneous techniques (except the Lowsley retractor technique), the patient should be supine. Also, the patient should always be in the Trendelenburg position. This allows the bowels to fall cranially, decreasing the likelihood of puncturing the gastrointestinal tract during catheter placement. [7]
Monitoring and Follow-up
If not already under the care of a urologist, all patients who undergo suprapubic tube placement should be referred to a urologist for correction of the underlying disease, as well as routine cystostomy tube care.
The first catheter change should take place after approximately 4-6 weeks to allow time for a tract to form. Subsequently, if the catheter is intended for long-term use, it can be changed monthly, with upsizing (eg, to a lumen of 22 or 24 French) if desired. Any lumen smaller than 16 French in diameter is at high risk for obstruction (with sediment or mucus) over time. Repeated catheter blockage should be investigated with cystoscopy. [2]
Some patients may require additional procedures, such as revision of the suprapubic catheter site, surgical closure of the bladder neck or urethra, procedures for treatment of calculi, or anticholinergic medication to stop bladder spasms that might be associated with urethral leakage. Over an extended period, long-term indwelling catheters are associated with chronic inflammation of the urothelium, with a small increased risk of bladder malignancy over years. [8] Thus, annual screening cystoscopies should be considered in this patient population.
-
Suprapubic cystostomy placement under cystoscopic guidance.
-
An example of the Cook Peel-Away Sheath set.
-
An example of the Stamey percutaneous cystostomy set.
-
Algorithm for managing difficult-to-catheterize patient. Arrows indicate next reasonable step; horizontal lines indicate that either option is reasonable.
-
Erosion of ventral surface of penis. Foley catheter has eroded glans, penile skin, and almost entire penile urethra. (Reprinted from Vaidyanathan S, Soni BM, Hughes PL, et al. Severe ventral erosion of penis caused by indwelling urethral catheter and inflation of Foley balloon in urethra. Adv Urol. 2010; 461539.)
-
Gross anatomy of the bladder.