Scleroderma, also called systemic sclerosis, is an autoimmune disease that affects the skin and some internal organs of the body. The body’s immune system damages normal, healthy tissues and replaces them with scar tissue, causing thickening and tightening of the skin. The name scleroderma comes from two Greek words: “sclero” means hard and “derma” means skin.
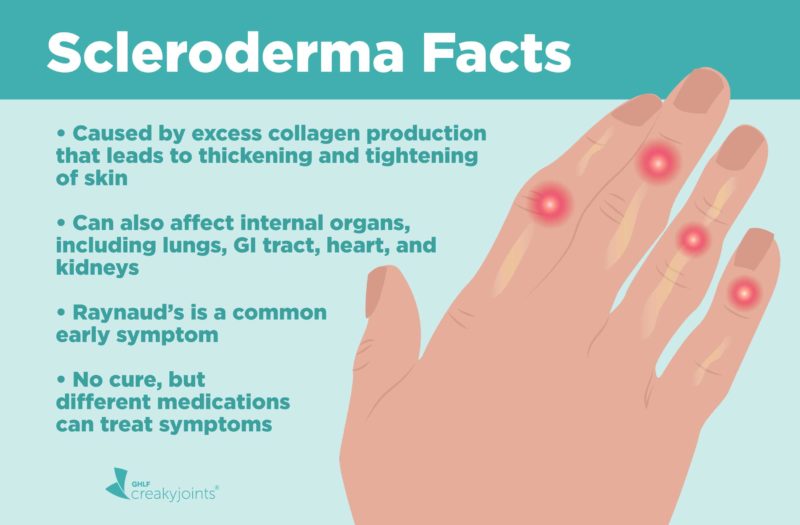
When a person has scleroderma, the body makes too much collagen, which is a fibrous protein that makes up your body’s connective tissues, including your skin. Excess collagen cause hardening and tightening.
Most people with scleroderma have hardening and tightening of their skin, but joints, muscles, and even internal organs like the lungs and blood vessels can be affected.
Inflammation and scarring (called fibrosis) from scleroderma can damage organs and systems throughout the body, including the lungs (interstitial lung disease), heart (heart failure or heart rhythm problems), and gastrointestinal tract (motion problems throughout intestine). Blood vessels may also be involved, causing serious complications including pulmonary arterial hypertension (blood pressure in the blood vessels going to the lungs is too high) and scleroderma renal crisis, where severe high blood pressure can cause kidney disease.
Scleroderma affects about 75,000 to 100,000 people in the United States, according to the American College of Rheumatology (ACR). It affects women more often than men and most commonly first occurs between ages 30 to 50. But because scleroderma is not exactly a household name, people who start to develop symptoms may take a long time to get diagnosed, or they may be misdiagnosed as having other issues like rheumatoid arthritis or lupus.
In fact, even some primary health care providers can be unaware of the symptoms of scleroderma. That’s why improved awareness among both patients and primary care physicians is needed for earlier diagnosis, says a study in the journal Rheumatology.
There is no cure for scleroderma. Current treatments address managing specific symptoms rather than preventing disease progression. Research focused on better treatments is ongoing and promising. Health care providers who treat scleroderma, such as rheumatologists, work closely with patients and other specialists to monitor for complications and help scleroderma patients stay as healthy as possible.
According to the American College of Rheumatology, “the effects of scleroderma vary widely and range from minor to life-threatening, depending on how widespread the disease is and which parts of the body are affected.”
Types of Scleroderma
There are two general types of scleroderma: localized and systemic.
Localized scleroderma
Localized scleroderma generally is limited to the skin, although it can affect the bones and joints. Localized scleroderma does not affect internal organs like the lungs or kidneys. It can cause hard, discolored, oval-shaped patches on the skin called morphea, or linear streaks of thickened, hard skin called linear scleroderma.
This kind of scleroderma may be misdiagnosed as rheumatoid arthritis or other conditions, says Ali Ajam, MD, a rheumatologist at The Ohio State University Wexner Medical Center in Columbus. When it comes to the joints, many autoimmune conditions present similarly, he says. Joint stiffness and swelling are common manifestations that tend to be synonymous with all these conditions.
Systemic scleroderma
Systemic scleroderma is often called systemic sclerosis. It affects skin and internal organs through inflammation and scarring, says Zsuzsanna McMahan, MD, assistant professor of medicine in the division of rheumatology at Johns Hopkins Scleroderma Center in Baltimore, Maryland. This multi-system autoimmune disease is defined based on the extent of skin involvement and other factors, says Lindsay S. Lally, MD, rheumatologist at Hospital for Special Surgery in New York City.
There are two main kinds of systemic sclerosis, according to the Scleroderma Foundation:
Limited cutaneous scleroderma (formerly called CREST syndrome)
The name CREST syndrome comes from symptoms that people with limited cutaneous scleroderma have:
- Calcinosis: Painful lumps of calcium in the skin that can happen on your fingers or other parts of your body
- Raynaud’s phenomenon: White or cold skin on the hands and feet when you’re cold or stressed that’s caused by blood flow problems
- Esophageal dysfunction: Problems swallowing and/or reflux caused by scarring in the esophagus
- Sclerodactyly: Tightness and thickening of finger or toe skin that can make it hard to bend your fingers
- Telangiectasias: Red spots on the hands, palms, forearms, face, and lips caused by widened blood vessels
CREST syndrome was used to describe limited cutaneous scleroderma before it was realized that patients also had internal organ involvement, says Virginia Steen, MD, a professor in the division of rheumatology in the department of medicine at Georgetown University Medical Center in Washington, D.C.
Patients with limited cutaneous scleroderma have skin thickening that is restricted to fingers, hands, forearms, legs, and feet. They usually have Raynaud’s disease, where fingers and toes are sensitive to the cold and become white or blue (gray) in the cold, and sometimes puffy fingers for a long time before other problems develop, says Dr. Steen. They can have digestive involvement and interstitial lung disease, but this is less common than in diffuse scleroderma. They rarely get kidney problems, but they have a higher frequency of pulmonary hypertension, which can develop in up to 15 to 20 percent of cases, she says.
Diffuse cutaneous scleroderma
This more serious form of systemic sclerosis may progress quickly. Skin involvement often includes more of the body, including the trunk, and other internal organs are more commonly involved (kidneys, blood vessels, GI tract). Interstitial lung disease and kidney problems are more common than in limited cutaneous scleroderma.
Causes of Scleroderma
Anyone can get scleroderma, though it impacts more women than men. It’s unknown exactly what causes scleroderma, though it results from the immune system attacking your own body, causing an overproduction and accumulation of collagen in body tissues, says Dr. McMahan. Genetic and environmental factors likely play a part in determining the risk of developing this condition.
Family history
Twins and family members of those with scleroderma or other autoimmune connective tissue diseases, such as lupus, may have a slightly higher risk of getting scleroderma. But most cases of scleroderma are sporadic and occur in people with no family history of the disease.
Environmental factors
Environmental exposures like silica in men (which was seen in in the past in coal and gold miners) and certain chemicals may affect the risk of developing scleroderma. But the majority of people with scleroderma do not have a history of exposure to any suspicious toxins, says the American College of Rheumatology.
“It may be that different patients have different triggers,” says Robert Spiera, MD, a rheumatologist and director of the Vasculitis and Scleroderma Program at the Hospital for Special Surgery in New York City. “The underlying cause, however, is unknown.”
Symptoms of Scleroderma
Signs and symptoms vary depending on which type of scleroderma you have. People vary greatly in how their illness progresses and changes over time. A study in the journal Rheumatology found that the most common symptoms in terms of frequency and moderate-to-severe impact on daily activities for study participants with systemic sclerosis were fatigue, hand stiffness, joint pain, and difficulty sleeping.
Pain
In the beginning, many people experience puffy, swollen fingers that become very sensitive to cold, and/or fingers that may change color when exposed to cold or stress. For many people, these are the first hint of scleroderma. Your fingers may also feel tight, like something is pulling on them, says Dr. Ajam.
Stiffness and swelling
Many scleroderma patients have hand stiffness and swelling that is worse in the morning and improves with activity throughout their day. Swelling is usually not just in the joints or knuckles; the whole hand and finger can look puffy, swollen, tender, inflamed, and uncomfortable. It can be difficult to make a tight fist, tie shoes, and button buttons.
Raynaud’s disease
Approximately 85 percent to 95 percent of systemic sclerosis patients experience Raynaud’s disease, according to the Cleveland Clinic. In fact, Raynaud’s is one of the earliest signs of scleroderma. It causes the small blood vessels in your fingers and toes to contract or spasm when it is cold or you’re under stress. They may turn blue and then white and feel painful or numb. In severe Raynaud’s cases, ulcers can form because of poor blood flow.
Skin thickening, darkening, and tightening
Nearly everyone with scleroderma has some thickening of the skin. It often starts on the fingers and feet and moves up the arms or legs. If the scleroderma is diffuse, it will also involve the upper arms/legs and trunk. Patients have a darkening, hardening, thickening, and tightening of patches of skin. Patches can be purplish at the edges and may be shaped like ovals or straight lines, says Kenneth Beer, MD, a dermatologist who is affiliated with Good Samaritan Medical Center in West Palm Beach, Florida. They may cover wide areas of the trunk and limbs. The number, location, and size of patches vary by the type of scleroderma. Skin can look shiny and movement may be restricted in the affected area. Muscles and tendons can also be involved, causing pain and weakness.
Heartburn, difficulty swallowing, and other GI issues
Scleroderma can impact all parts of the GI system, “but it most commonly affects the esophagus,” says Dr. Ajam. Strictures (narrowing or tightening) can develop in the esophagus, making it difficult to swallow and causing heartburn, acid reflux, and bloating. Rarely, you can have blood loss from inflammation or irritation in the GI system, says Dr. Steen.
Some people have problems absorbing nutrients if the intestinal muscles aren’t moving food properly through the intestines. Motility problems can also lead to chronic diarrhea. Intestinal blockages can be a severe complication that usually requires hospitalization.
Scleroderma Lung and Kidney Complications
Lungs
These organs can be affected by scleroderma in varying degrees. Two types of lung disease may develop in those with scleroderma.
Interstitial lung disease is associated with scarring of the lung tissue. Immunosuppressive medications such as cyclophosphamide and mycophenolate are somewhat effective in treating the interstitial lung disease in scleroderma. Clinical trials have shown that these drugs improve lung functions and symptoms in scleroderma. Nintedanib (Ofev) was FDA-approved in 2019 as a treatment for systemic sclerosis-associated interstitial lung disease (SSc-ILD). Previously approved to treat idiopathic pulmonary fibrosis, nintedanib is the first treatment specifically for SSc-ILD.
Pulmonary arterial hypertension, or high blood pressure in the arteries in the lungs, is the second type of lung disease seen in scleroderma. This complication of scleroderma happens when the pressure on the right side of your heart increases, causing it to wear out, says Dr. McMahan. Early symptoms of pulmonary hypertension include shortness of breath, chest pain, and fatigue.
Drugs are recommended to open the blood vessels in the lungs. Medications include prostacyclin-like drugs (epoprostenol, treprostinol, iloprost), endothelin receptor antagonists (bosentan, ambrisentan), and PDE-5 inhibitors (sildenafil, vardenafil, tadalafil) — also used to treat erectile dysfunction.
“These drugs have now turned a once-fatal complication into a very serious, but treatable, one,” says Dr. Steen.
Kidneys
Some patients with diffuse cutaneous scleroderma experience scleroderma renal crisis (SRC), says Dr. Lally. SRC is characterized by sudden hypertension (high blood pressure) and rapidly progressive kidney failure, hypertensive encephalopathy (brain dysfunction due to high blood pressure), congestive heart failure, and/or microangiopathic hemolytic anemia (loss of red blood cells).
It’s more common in patients who are treated with glucocorticoids (a class of corticosteroids); the risk rises with increasing steroid doses.
Scleroderma renal crisis can be treated with a type of blood pressure medication called ACE inhibitors. But if the condition goes unrecognized, it can quickly lead to kidney failure and the need for dialysis. Dr. Ajam says he used to see the condition more before today’s treatments were in place.
How Scleroderma is Diagnosed
Scleroderma can be difficult to diagnose because it can manifest in many forms and impact many areas of the body. Symptoms may be similar to other diseases.
Physical exam and medical history
Your doctor will do a physical exam and take a history of your symptoms. In the exam, the doctor will look for skin tightening or swelling. They may order a biopsy to view a small sample of the affected skin.
Blood tests
While no blood test can definitively confirm that you have scleroderma, they can reveal elevated levels of certain antibodies that are common in some forms of scleroderma, including anti-nuclear antibodies, which are present in about 95 percent of people with systemic sclerosis.
Lung function and imaging tests
Pulmonary function tests are done to measure how the lungs are functioning. If scleroderma is suspected, doctors want to know whether it has spread to the lungs, where it can cause scar tissue formation. Such breathing tests can measure how well the lungs are working. An X-ray or CT scan can also show evidence of lung damage.
Other tests
Additional testing may be needed to help determine the extent to which scleroderma is affecting internal organs. An EKG or electrocardiogram can see if the heart damage from scleroderma. X-rays and MRIs can show changes in the bones or soft tissues. An endoscopy can be done to look for involvement in the stomach, intestines, and esophagus. A manometry can specifically measure the strength of the esophageal muscles. Blood and urine tests can assess test kidney function. When scleroderma affects the kidneys, it can increase blood pressure as well as leakage of protein into the urine.
How Scleroderma Is Treated
There are currently no medications to cure or stop the overproduction of collagen associated with scleroderma. But several therapies are currently being evaluated in clinical trials to address these issues, says Dr. McMahan. Other medications are used to help control scleroderma symptoms and prevent complications.
Topical creams
Some of the same topical treatments used for eczema, psoriasis plaques, or other skin growths, including calcipotriene, topical steroid creams, imiquimod, and tacrolimus ointment may help treat morphea patches from scleroderma.
Phototherapy
UV light therapy and laser treatments can be used for more severe cases where the morphea patches go deeper or are very extensive on the skin.
Medications to dilate blood vessels
Blood pressure medications that dilate blood vessels may help treat Raynaud’s disease in scleroderma. Calcium channel blockers such as nifedipine (Procardia) or amlodipine (Norvasc) are a first-line treatment for Raynaud’s. When that is insufficient to control Raynaud’s, phosphodiesterase inhibitors like sildenafil (Viagra) may be helpful, says Dr. Lally.
Scleroderma renal crisis is specifically treated with ACE inhibitors.
Nitrates
To improve blood flow so that finger sores can heal, some doctors may recommend nitrates such as nitroglycerin. This medication relaxes the smooth muscles (ones that form the blood vessels and some organs), causing arteries to dilate.
Antacids
Antacids can help with GI-related symptoms like acid reflux and heartburn. Doctors may prescribe proton pump inhibitors (PPIs) like omeprazole (Prilosec), iansoprazole (Prevacid), pantoprazole (Protonix), or esomeprazole (Nexium), or H2 receptor blockers like ranitidine (Zantac) or famotidine (Pepcid). PPIs decrease acid production in the stomach. H2 receptor blockers block histamine, a chemical that promotes acid production in the stomach.
Sucralfate (Carafate) is sometimes prescribed to help coat stomach ulcers, which can improve healing, says Dr. Lally. Systemic scleroderma patients with slow gastrointestinal motility (where food moves too slowly through the digestive tract) may benefit from medications that enhance motility like metoclopramide (Reglan) or prucalopride (Prudac), says Dr. McMahan.
Immunosuppressive medications
Immune-suppressing drugs such as methotrexate and mycophenolate mofetil (CellCept) are used to help treat skin thickening. Cyclophosphamide and mycophenolate mofetil have also been shown to improve lung function and symptoms, Dr. Steen says.
Physical and occupational therapy
Physical and occupational therapists can help manage pain and improve strength, flexibility, and mobility so you can perform daily tasks. “Movement is key any time you’re dealing with inflammation,” says Dr. Ajam.
Occupational therapy often focuses on the hands, since people with scleroderma have issues with grip strength. Therapists may fashion splints or braces to improve function and reduce the likelihood of the development of digital ulcers (open sores on fingertips).
Exercise
Staying active, such as with low-impact cardio exercise, stretching, and strength training, can help keep your body flexible, improve strength and circulation, and relieve stiffness. Range-of-motion exercises can keep skin and joints flexible. If you have pulmonary or cardiac involvement, discuss your exercise regimen with your doctor before you start, Dr. Lally adds.
Skin care and protection
Proper skin care can help Raynaud’s and thick skin. Avoid very hot baths and showers as well as strong soaps, cleaners, and household chemicals, which can irritate and dry out your skin. Use sunscreen to protect your skin. “You don’t want to burn your skin and cause more scarring,” says Dr. Beer.
Use moisturizing creams or lotions, emollients, or petroleum jelly after bathing to soothe skin. “They can manage itchiness and dryness associated with scleroderma,” says Dr. Ajam. Consider setting up a humidifier to help keep the air in your home moist.
Smoking cessation
Nicotine can cause blood vessels to contract, worsening Raynaud’s disease. It can also cause permanent blood vessel narrowing and worsen lung problems.
GI-friendly diet
Foods known to exacerbate reflux include spicy fare, citrus fruits, tomato-based products, and caffeine, says Dr. Lally. Try not to eat late at night and eat small meals more frequently since your GI system can’t handle digesting a lot of food at once.
Staying warm
When you’re exposed to the cold — and not just cold weather outdoors, but environments with a lot of air conditioning or places like grocery-store frozen-food sections — dress appropriately. Hand and feet warmers may be helpful. Carry gloves with you to use as needed. Footwear should be loose fitting to keep the blood supply moving to your feet. “Keeping your extremities and core warm in the cold weather is crucial for managing Raynaud’s,” says Dr. Lally.
Surgery
Surgical options are a last resort for scleroderma complications. “Rarely do we get to the point that you require surgery,” says Dr. Ajam. Those with severe interstitial lung disease or pulmonary hypertension may be candidates for a lung transplant. Kidney transplant may also an option for those with end-stage renal disease related to scleroderma renal crisis.
Emerging Treatments for Scleroderma
Stem cell transplants are a rich area of research interest. In this procedure — commonly used to treat certain blood cancers, like leukemia — your own stem cells (which can develop into different types of cells) are removed and the body’s immune system is “wiped out” with chemotherapy and radiation. The stem cells are then returned to the body, where they rebuild the immune system. It is risky, especially soon after treatment begins, because there is a period where the immune system doesn’t function well enough to protect you from infections. In a trial published in 2018 in the New England Journal of Medicine 36 people with severe scleroderma received stem cell transplantation and were compared with 39 similar people who received a year of standard immune-suppressing medication. After 4.5 years, those assigned to receive stem-cell transplantation had improved overall survival (without serious lung, kidney, or heart complications) compared with standard treatment and less need for immune-suppressing medication. More research on larger patient populations is needed.
Researchers are also continuing to study the use of intravenous immunoglobulin (IVIG) to treat scleroderma, which has had a lot of positive observational studies but now will be in a large clinical trial, says Dr. Steen. IVIG is made up of antibodies and is sometimes used to treat various autoimmune conditions.
Rituximab (Rituxan) is a biologic medicine — already used to treat many other conditions, such as rheumatoid arthritis and non-Hodgkin’s lymphoma — that is currently being investigated to treat people with systemic sclerosis with interstitial lung disease.
Several other trials of new medications that target specific pathways involved in scleroderma are in early stages:
Lenabasum is an oral medication considered a first-of-its-kind treatment because it is a cannabinoid-related drug. It targets the signaling system that cells use to resolve or turn off inflammation without suppressing the immune system as a whole. “It’s now in phase 3 trials and we are very excited about this,” says Dr. Steen.
Researchers are studying a drug that inhibits immune system components called TGF beta, which are thought to play a role in the fibrosis that occurs in systemic sclerosis.
Data presented at the 2019 American College of Rheumatology/Association of Rheumatology Health Professionals Annual Meeting showed that patients with scleroderma who were treated with romilkimab, a biologic that inhibits immune system proteins interleukin 4 (IL-4) and interleukin 13 (IL-13) showed a statistically significant improvement in skin thickening compared to those who received a placebo.
“There is lots of hope for the future treatments of scleroderma,” Dr. Steen says.
Join ArthritisPower
If you are diagnosed with scleroderma or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Keep Reading
Allanore Y, et al. Efficacy and Safety of Romilkimab in Diffuse Cutaneous Systemic Sclerosis (dcSSc): A Randomized, Double-Blind, Placebo-Controlled, 24-week, Proof of Concept Study [abstract]. Arthritis & Rheumatology. 2019. https://acrabstracts.org/abstract/efficacy-and-safety-of-romilkimab-in-diffuse-cutaneous-systemic-sclerosis-dcssc-a-randomized-double-blind-placebo-controlled-24-week-proof-of-concept-study.
Bassel M, et al. Frequency and impact of symptoms experienced by patients with systemic sclerosis: results from a Canadian National Survey. Rheumatology. April 2011. doi: https://doi.org/10.1093/rheumatology/keq310.
Distler O, et al. Factors influencing early referral, early diagnosis and management in patients with diffuse cutaneous systemic sclerosis. Rheumatology. February 2018. doi: https://doi.org/10.1093/rheumatology/kex504.
Forbius Announces the First Patient Dosed in a Phase 1b Diffuse Scleroderma Trial of AVID200, a Novel TGF-beta 1 & 3 Inhibitor. Forbius. https://forbius.com/press-releases/forbius-announces-the-first-patient-dosed-in-a-phase-1b-diffuse-scleroderma-trial-of-avid200-a-novel-tgf-beta-1-3-inhibitor.
Interview with Ali Ajam, MD, rheumatologist at the Ohio State University Wexner Medical Center
Interview with Kenneth Beer, MD, Beer Dermatology
Interview with Lindsay S. Lally, MD, rheumatologist at the Hospital for Special Surgery
Interview with Robert F. Spiera, MD, Director of the Vasculitis and Scleroderma Program at the Hospital for Special Surgery
Interview with Virginia Steen, MD, rheumatologist at Georgetown University
Interview with Zsuzsanna McMahan, MD, rheumatologist at Johns Hopkins University
New Indication OK’d for Lung Drug Ofev. MedpageToday. https://www.medpagetoday.com/pulmonology/generalpulmonary/82029. Published September 6, 2019.
Patient education: Intravenous immune globulin (IVIG) (Beyond the Basics). UptoDate. https://www.uptodate.com/contents/intravenous-immune-globulin-ivig-beyond-the-basics.
Scleroderma. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Scleroderma.
Scleroderma. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/scleroderma/symptoms-causes/syc-20351952
Scleroderma: An Overview Management and Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8979-scleroderma-an-overview/management-and-treatment.
Scleroderma: Diagnosis and Treatment. American Academy of Dermatology. https://www.aad.org/diseases/a-z/scleroderma-treatment.
Sullivan KM, et al. Myeloablative Autologous Stem-Cell Transplantation for Severe Scleroderma. New England Journal of Medicine. 2018;378(1):35-47. doi: http://dx.doi.org/10.1056/nejmoa1703327.
Systemic scleroderma. Genetics Home Reference. U.S. National Library of Medicine. https://ghr.nlm.nih.gov/condition/systemic-scleroderma#inheritance.
What is Scleroderma? Scleroderma Foundation. https://www.scleroderma.org/site/SPageNavigator/patients_whatis.html#.XfQnuS_MzGJ.