Written by: Richmond Castillo, MD, MS, MA (NUEM ‘23) Edited by: Andra Farcas, MD (NUEM ‘21) Expert Commentary by: Matthew Kippenhan, MD
Expert Commentary
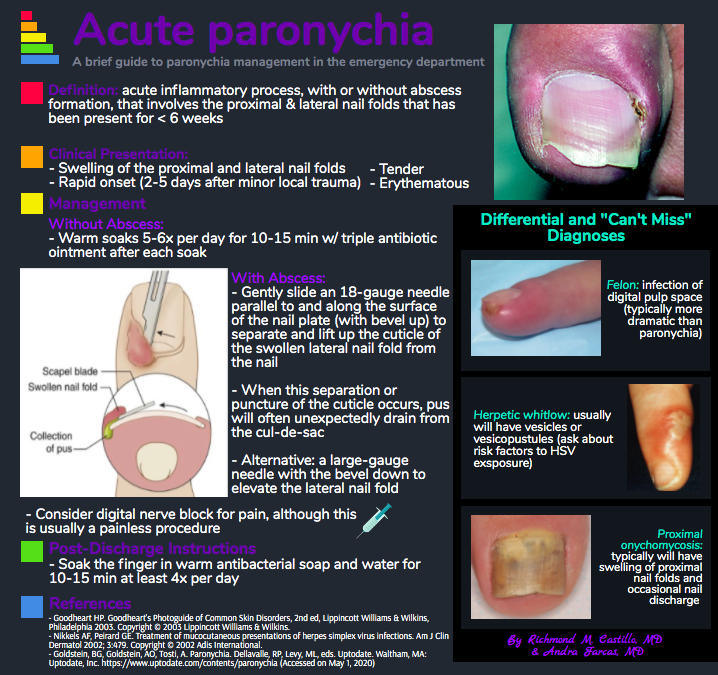
While paronychia is commonly seen in Urgent Care and Fast Track settings, this is a condition that some EM residents may not get much exposure to during their training. Knowledge of minor conditions such as this may not match the excitement of a critically ill patient, but it is an essential skill set for every EM physician.
The biggest pitfall I have seen in treating paronychia is failure to drain a patient who has a clear fluid collection. Providers not trained to perform the procedure will often give oral antibiotics as treatment, but once purulence has developed these will be ineffective without drainage. We tend to see a fair number of patients who have already been on antibiotics but have failed to improve.
If you see a patient without signs of abscess, provide proper instruction above on soaking and topical antibiotic ointment, but be sure to provide anticipatory guidance that it may still worsen and require drainage - just not yet. Patients appreciate knowing your thought process on why you are providing specific treatment based on their presentation.
When draining a paronychia, I prefer to use an 11 blade laid flat on the nail to make a small incision, then lifting the skin slightly away from the nail. While some tolerate the procedure well, I do offer a digital block to alleviate any apprehension. For those with more extensive involvement, you may place a wick with a short piece of 1/4" iodoform and have the patient remove it in 1-2 days. Be sure to offer a wound check in 48 hours - either in the ED or an urgent care if available. Counsel the patient that the finger will not look completely normal for 1-2 weeks but we want to see a steady improvement over that time.
Although infrequent, patients with diabetes or vascular disease can have further complications, such as an ascending cellulitis, evolution into a deep space infection of the digit, or even osteomyelitis. While the amount of pain typically drives patients to seek care sooner, patients with certain conditions (ie substance abuse, poor access to care, AMS) may go unrecognized for a longer period leading to more serious infection. Complicated cases like this should have imaging (xray) and consultation with a hand surgeon.
Matthew Kippenhan, MD
Medical Director, Emergency Department
Northwestern Memorial Hospital
Assistant Professor, Feinberg School of Medicine
Northwestern University
How To Cite This Post:
[Peer-Reviewed, Web Publication] Castillo, R. Farcas, A. (2021, Mar 1). Paronychia. [NUEM Blog. Expert Commentary by Kippenhan, M]. Retrieved from http://www.nuemblog.com/blog/paronychia.